Climate and Health: A Time Bomb
Climate change represents one of the greatest challenges in human history. It brings into question the right to health, which is a fundamental human right (WHO and Health Canada, 2021). According to the World Health Organization (WHO), climate change will cause an additional 250,000 deaths per year by the end of the current decade, due to malnutrition, malaria, diarrhea, and heat stress (WHO, 2014). Under these conditions, the implementation of public health adaptation measures is a priority if we are to protect the health and well-being of the population. This includes designing relevant and effective national adaptation plans (NAPs) (UNFCCC, 2015).
At the 26th Conference of the Parties in Glasgow in 2021, a number of countries pledged to make their health systems resilient to climate change as part of the Alliance for Transformative Action on Climate and Health (ATACH) (WHO, 2023). To help them achieve this, the WHO (2021) has defined quality criteria for Health National Adaptation Plans (HNAPs): 1) leadership and a suitable environment, 2) cross-sectoral coordination and policy coherence, 3) comprehensive treatment of climate-sensitive health risks, 4) comprehensive treatment of adaptation options and measures, 5) resource allocation and, finally, 6) monitoring, evaluation, and communication of results. The aim of this article is to present a comparative assessment of the NAPs submitted to the United Nations Framework Convention on Climate Change (UNFCCC) by different developing countries. This type of analysis highlights the similarities and dissimilarities, and above all the conformity of the content of these plans with accepted standards.
We begin with a definition of the concepts and a brief review of the links between health and adaptation. We then present the chosen methodological approach, before commenting on the results. Finally, we make some recommendations.
Human Health, Adaptation, and National Adaptation Plans
Health is “a state of complete physical, mental, and social well-being and not merely the absence of disease or infirmity” (WHO 1948). Climate change can therefore affect health in a number of ways. Physical health can be altered: the steady rise in Lyme disease in Canada, where the number of diagnosed cases has increased 1,844 % over the last decade, is a meaningful example (Government of Canada, 2022). Not to mention altered mental health due to stress, anxiety, and depression (WHO and Health Canada, 2021). Finally, on a social level, climate change hinders the achievement of sustainable development goals by exacerbating poverty and inequality, particularly for vulnerable populations and geographical areas (WHO and Health Canada, 2021).
To respond to the health impacts of climate change, it is crucial to assess the strengths and vulnerabilities of healthcare systems, in order to plan the modifications needed to increase their resilience2. With this in mind, we thought it would be interesting to study whether and how public health is taken into account in the process of national adaptation plans, with a view to making recommendations for their improvement.
Methodology
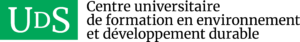
For the purposes of this article, we have chosen to include ATACH (Alliance for Transformative Action on Climate and Health) member countries, as this organization is, to our knowledge, the only emanation of a universal institution whose aim is to increase the resilience of health systems to climate change. The countries selected are those that have officially and freely committed to ATACH and have honoured this commitment by submitting a plan to the UNFCCC. They are Togo, Sierra Leone, Madagascar, Kenya, Ethiopia, Cape Verde, Central African Republic, Sri Lanka, Fiji, Liberia, Nepal, Burkina Faso, and the Democratic Republic of the Congo (Figure 1). Although the number of countries included is small, this methodology is relevant, as all are developing countries particularly vulnerable to the disastrous health consequences of the climate crisis.
We collected the health-related data from a careful and rigorous reading of the NAPs and added them to an Excel spreadsheet. For each content item corresponding to a quality criterion, we added a row to the spreadsheet and created a column for each country in order to visualize the results and create graphs and tables. Finally, we carried out an interpretative analysis of the results, which we present in the next section.
Results
Is Health Only the Fifth Priority for Adaptation?
Most of the NAPs analyzed (12/13) identified health as a priority and as a particularly vulnerable sector. However, while all the countries opted for a sector-by-sector approach in designing their plans, three of them did not devote a chapter to health, and on average, health only ranked fifth among the priorities. Table 1 summarizes the other results.
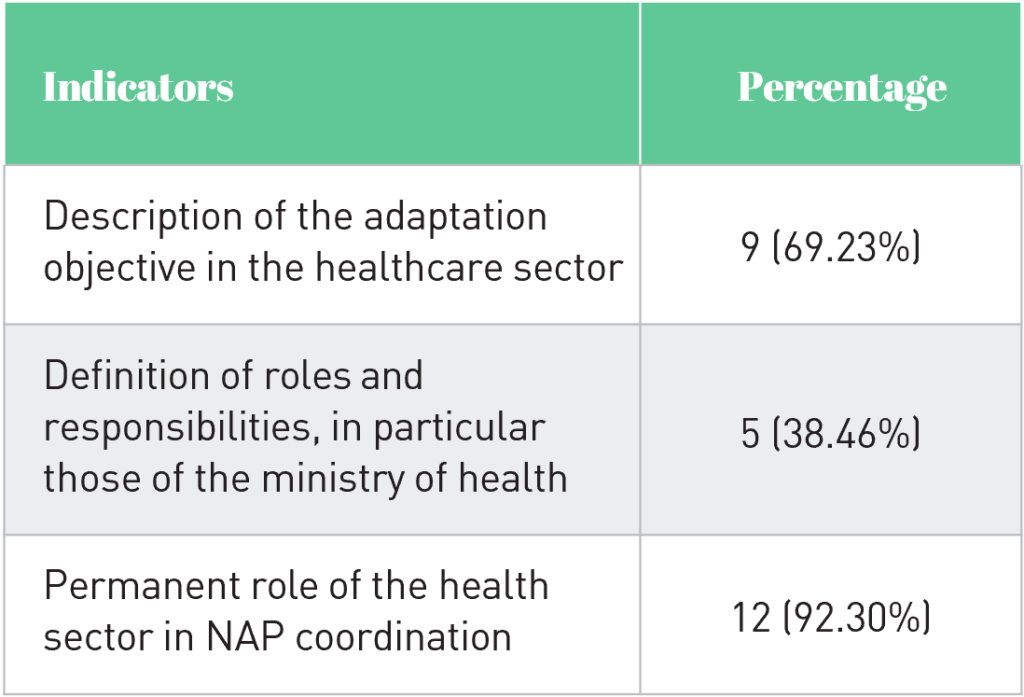
Among the countries that have presented their health adaptation objectives, some simply give the objectives of their national health policy in general terms (Togo). Others mention programs to combat the health impacts of climate change, with objectives for each program, without necessarily providing a global vision (Nepal). Still others present strategic objectives, described with the local context (Madagascar, Kenya, Ethiopia, Fiji, Burkina Faso). This overview shows that even when health adaptation objectives are mentioned, there are disparities in terms of precision.
None of the 13 NAPs analyzed achieved 100 % compliance with the identified indicators. This result might be explained by the fact that these countries are mostly developing and do not have sufficient technical resources to carry out the NAP development process. Progress remains to be made on several indicators, notably in terms of precision regarding needs, measures, and the role of health actors in adaptation policies. While we agree that a NAP devoted solely to health would have the merit of a higher level of precision, only the NAP of the Central African Republic mentions that an HNAP is under preparation. Finally, many health risks have not been considered in the NAPs analyzed, an issue we address in the next section.
Zoonoses and Mental Illnesses: The Great Neglected Aspect of Health Risk Assessment
Only 9 out of 13 NAPs provide a comprehensive assessment of the country’s vulnerability to health risks (Table 2). Moreover, for almost all of them, this assessment is very cursory, based on global rather than national data, and taking little account of the country’s specific situation.
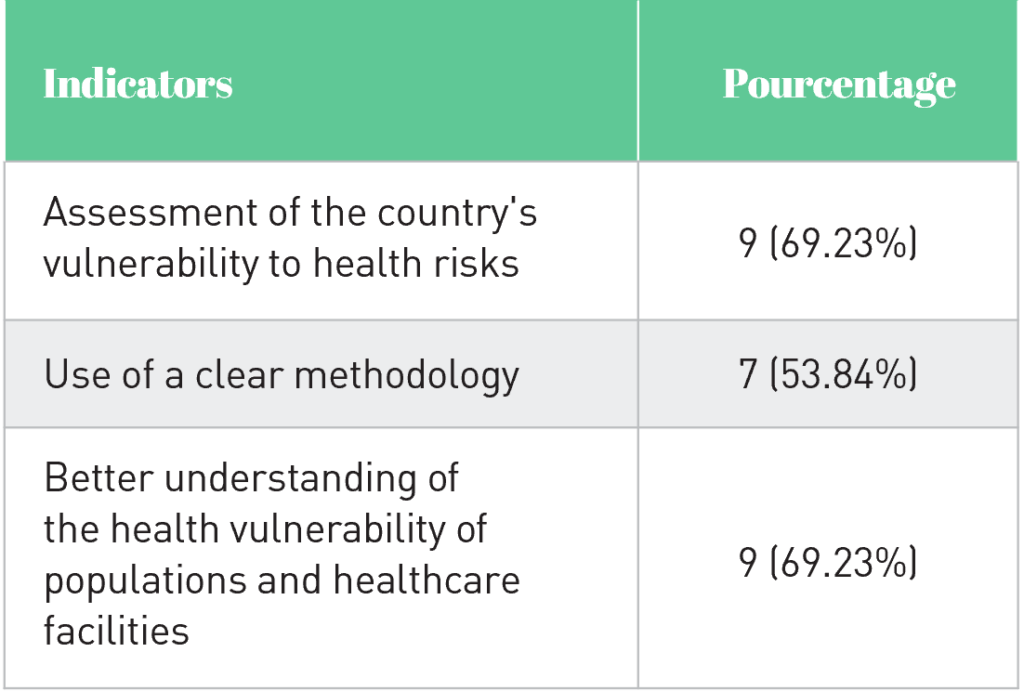
Several NAPs describe a methodology for assessing health risks (Madagascar, Fiji), providing a better understanding of vulnerability. However, most of the NAPs analyzed could be improved by using contextual data, establishing baselines and projections, and having a clear methodology. Similarly, the links between the choice of adaptation measures and the identified vulnerabilities would benefit from greater precision. These results can probably be explained by the fact that governments lack resources, expertise, and exhaustive data on health risks at the national level. The NAP for the Democratic Republic of the Congo is a good example of this issue. Indeed, the country’s plan explicitly recognizes the need for regular updates, and for human and institutional capacity building to increase research, analysis, and data management, and to fill existing gaps. The plan also recognizes the urgent need to produce information and vulnerability assessments that are useful for decision-making, using clear, organized, harmonized, and popularized methodologies. The same applies to Fiji’s NAP, which mentions informational, technological, institutional, financial, and economic barriers to NAP implementation. This is particularly important since, without the means to overcome them, these barriers can relegate health to the background in adaptation policies.
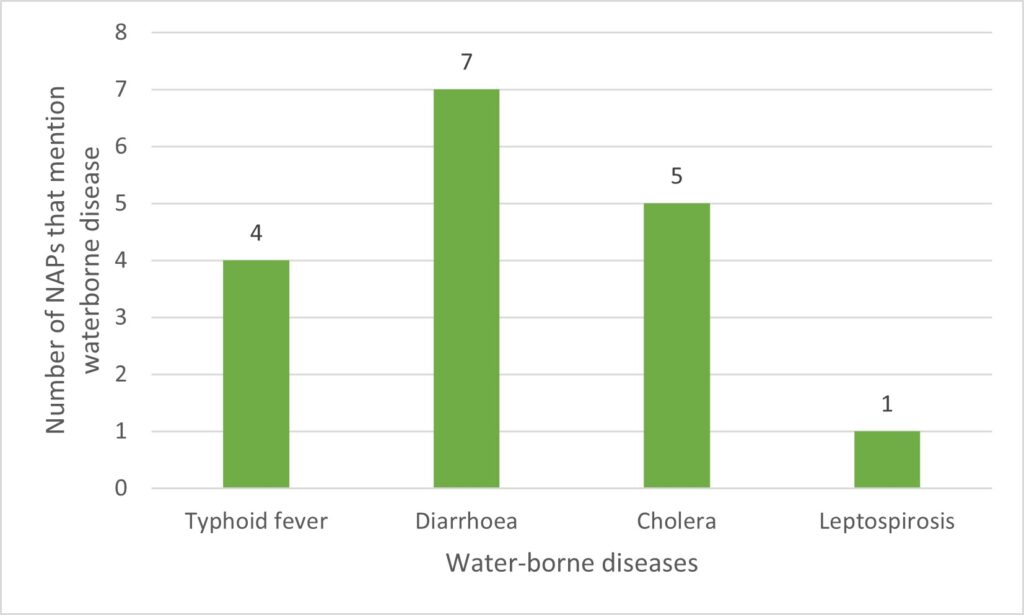
In addition to the shortcomings mentioned above, all the plans mention climate-related health risks. Our analysis shows that the risks most frequently mentioned are vector-borne and waterborne diseases. Figures 2, 3, and 4 show the distribution of climate-sensitive health risks found in the NAPs.
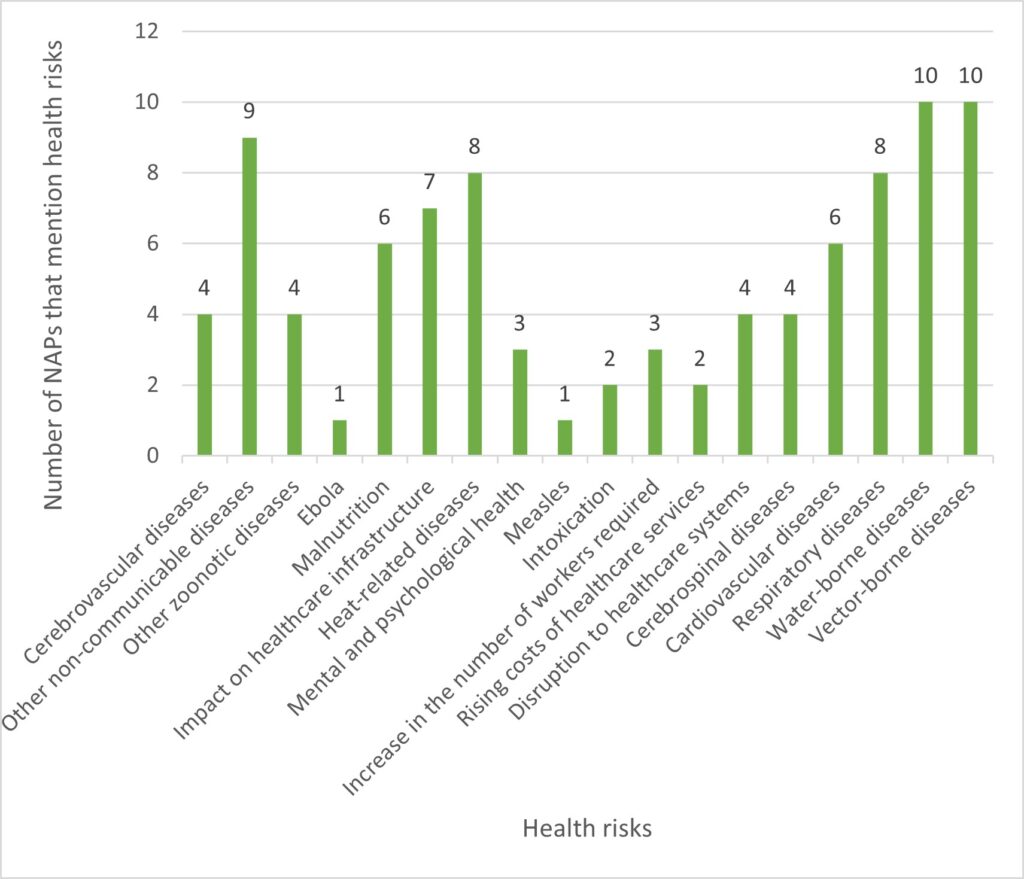
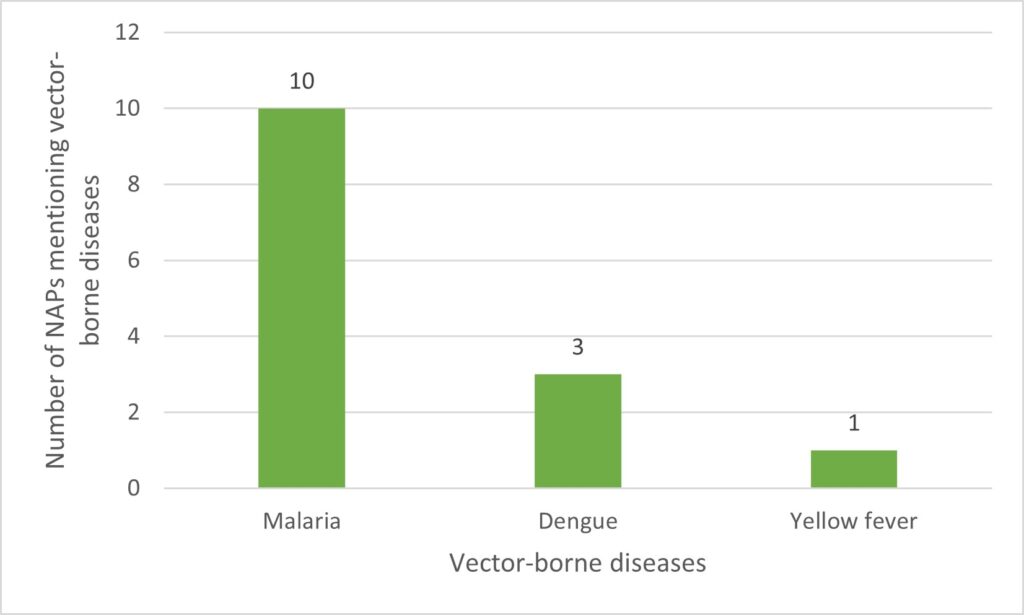
These results show that zoonoses and mental illnesses are among the health risks least represented in NAPs. This is paradoxical, considering the upsurge in zoonoses in recent years in most of these countries, and the numerous epidemics currently underway (WHO, 2022). Similarly, the ravages of mental illness linked to extreme weather phenomena and other manifestations of climate change are given very little consideration in these NAPs. Think, for example, of the climatic migrations linked to the destruction of the homes, living environments, and economic activities of the inhabitants of these countries, particularly those in disadvantaged rural areas. These events are vectors of numerous mental illnesses that represent a major public health problem.
The identification of health risks must be followed by the definition of adaptation measures to address them. In the next section, we analyze the suitability of the measures presented in the NAPs for the risks identified.
Insufficient adaptation measures
Ideally, HNAPs should contain adaptation options for the medium and long terms. Figure 5 shows the distribution of the main health-related adaptation measures in relation to the risks identified.
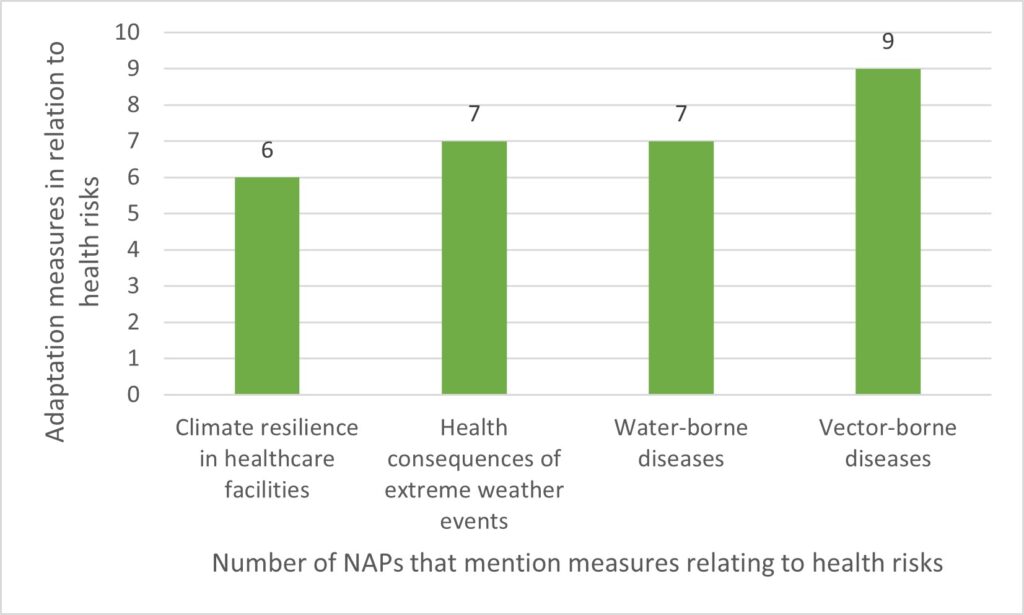
In the NAPs analyzed, the measures chosen concerned, for example, strengthening disease surveillance, prevention, and treatment, and stepping up scientific research (Burkina Faso, Cape Verde), improving access to drinking water (DRC), modelling disease incidence (Sri Lanka), building climate-resilient healthcare infrastructures (Ethiopia, Nepal), and strengthening early warning systems (Madagascar). However, there is a gap between the climate risks identified and the specific measures chosen to address them. For example, six NAPs mention malnutrition as a climate-sensitive disease, but only half propose adaptation options to address it. Similarly, of the ten NAPs that identify water-borne diseases, only seven mention measures to address them. Finally, the response to zoonoses and mental illnesses is virtually non-existent in these measures.
In our study, all the NAPs mention specific population groups as priorities for health adaptation measures. These are mainly rural populations (11), women (10), people with low incomes (10), young people (9), and people with disabilities (8). In order to protect the health of these vulnerable populations, WHO suggests that measures identified in NAPs take into account health co-benefits, provide sufficient resources for implementation, and be subject to periodic evaluation.
Little Mention of Co-Benefits, Inadequate Resources, and Monitoring
We identified only three NAPs (Sierra Leone, Madagascar, Cape Verde) that clearly demonstrate the health co-benefits of measures taken in other sectors. Similarly, only eight NAPs have calculated the budget required to implement health adaptation measures, corresponding to an average of $67.5 million. Finally, only three NAPs have defined indicators for monitoring progress in health adaptation (Ethiopia, Sri Lanka, Burkina Faso). Sri Lanka, for example, has identified as an indicator the number of research studies carried out on the links between health and the climate crisis.
Recommendations
A limitation of our research is the heterogeneity of the NAPs in terms of structure and methodology, making the analysis tedious. This limitation was overcome by careful reading of the NAPs, rigorous data collection and systematic interpretative analysis of the results, on the basis of which we make the following recommendations:
Recommandation 1: Set up an international mechanism to provide technical expertise to countries in the NAPs development process.
Recommandation 2: Increase ministry of health involvement in NAP processes, to improve understanding of the health consequences of the climate crisis and how they can be considered.
Recommandation 3: Improve NAPs through comprehensive identification of health risks, contextual data, and coherent health adaptation measures.
Recommandation 4: Plan a strategy for mobilizing the resources and funds needed to implement measures and to remove informational, technological, and institutional barriers.
The author was awarded the excellence scholarship from Regroupement étudiant de maîtrise, diplôme et doctorat de l’Université de Sherbrooke (REMDUS)
It is the capacity of a human community or health system exposed to hazards
to withstand, absorb, adapt to, transform, and recover from their negative impacts quickly and effectively (WHO and Health Canada, 2021).